Paper 14.4 Evaluating Allergen Information for Non-Prepacked Foods: Best Practise Guidance
On this page
Skip the menu of subheadings on this page.Summary
This paper summarises current work around the provision of allergen information for non-prepacked food, including the policy context for new best practice guidance for food business operators (FBOs), and the initial thinking around evaluation approaches. This paper is for information and discussion.
Members are asked to consider:
1. Is anything missing from the theory of change? Are there any problematic assumptions and/or any evidence gaps?
2. Does the proposed evaluation approach address the research aims? What else could we do to inform our understanding of the effectiveness of the best practice guidance?
Background
The FSA Food Hypersensitivity Strategy aims to improve the quality of life for people living with food hypersensitivities (allergies, intolerance and coeliac disease) and support them to make safe, informed food choices to effectively manage risk. This vision is set out in seven objectives across three key themes: safety, trust and choice.
On 5th March 2025, the FSA published new best practice guidance on the provision of allergen information for non-prepacked foods[1]. This guidance will apply in England, Wales and Northern Ireland. Under current legislation, food business operators (FBOs) are required to provide consumers with information on the 14 regulated allergens, but have a choice about whether they provide this information in writing or verbally. The new guidance sets out how FBOs can provide this mandatory allergen information to consumers. The guidance is intended to support businesses to comply with regulations in the most effective ways and meet consumer expectations by adopting good practices.
The guidance is for all FBOs selling non-prepacked foods[2], including distance sellers, and makes 8 key recommendations:
1. FBOs who provide non-prepacked foods should make information on the 14 regulated allergens easily available in writing to consumers.
2. Written allergen information should be supported by a conversation with the consumer and FBOs should encourage consumers to make them aware of any allergen requirements.
3. FBOs should display a message (e.g. on menus or signs) to let consumers know how to find allergen information and to encourage them to tell staff of any allergen requirements, if:
- they do not provide written allergen information upfront, and/or
- they do not routinely ask about allergen requirements.
4. FBOs should keep a record of the full ingredients in their dishes (if this information is available to them), so they can tell consumers if other allergens are present in their food if asked.
5. Staff should receive training on allergens and food hypersensitivity.
6. FBOs should have processes in place to ensure that consumer allergen requirements are accurately recorded, shared in writing with the person preparing the food and understood.
7. Food that has been prepared to meet allergen requirements should be easily identifiable (e.g. by a label) for the person serving the food and the consumer receiving it, and servers should also give verbal confirmation that the food meets allergen requirements.
8. Distance sellers should:
- Make written allergen information available to consumers before food is ordered, or provide it verbally over the phone.
- Ask consumers about allergens when they place their order.
- Provide written confirmation of allergen information on delivery
In December 2023, the FSA Board agreed that allergen information should be provided in writing and that this should be supported by a conversation between the business and the consumer. The guidance was created to encourage this. The Board also proposed that they would like the FSA to explore how requiring written allergen information could be underpinned by legislation.
As a non-ministerial department, we do not have the power to decide whether legislation should be introduced. However, we are currently gathering evidence and assessing the impact of different legislative options to inform any future Ministerial decision. Evidence around the effectiveness of the guidance will provide key considerations for this decision. Given we do not know the timings for this decision, and are keen to provide useful insight at various stages of the decision making process, we propose a range of evaluation activities to enable emerging/interim findings to be considered.
[1] Non-prepacked food refers to food which is not in manufacturer’s packaging at the point of sale. This includes food sold from delicatessen counters, loose fruit and vegetables and loose baked goods, as well as food sold in the catering or food services sector (e.g. restaurant and takeaway meals).
[2] Food that is prepacked for direct sale (PPDS) must follow allergen labelling regulations, also known as Natasha's Law, and be labelled with a full ingredients list, with allergenic ingredients emphasised within the list.
Evaluation research questions
The overarching aim of evaluation is to explore:
- Impacts (if any) of the best practice guidance on food business practices and on consumers with food hypersensitivities
- Considerations for possible future legislation
The evaluation will aim to answer the following research questions:
- Are FBOs following the best practice guidance?
- What are the barriers to and enablers of implementation? How, if at all, have FBOs adapted their practices to follow the guidance, and what impact has this had on businesses?
- How, if at all, have FHS consumers’ experiences of buying non-prepacked food changed since the introduction of the guidance? For example: has access to allergen information improved, do consumers feel more confident when buying non-prepacked food, and do they have more trust in how allergen information is communicated to them?
- Are FHS consumers experiencing fewer ‘near misses’ and adverse reactions from non-prepacked food?
- Have there been any unintended consequences (positive or negative) for FBOs or consumers following the introduction of the guidance?
Proposed evaluation approach
We are interested in both a process and outcome evaluation of the best practice guidance, to explore how it is being implemented and any changes that it may have led to. We are not able to employ an experimental design (due to policy timeframes and coverage) and so will not be able to attribute causality. Findings will be caveated accordingly.
As set out below, we propose a mixed methods approach, allowing us to provide insights at various stages to inform discussions round the need for legislation.
We commissioned baseline surveys of FBOs (n=520) and consumers (n=780 adults with FHS and n=180 parents of children with FHS) in England, Wales and Northern Ireland, to understand experiences and practices ahead of the guidance launch. Whilst we have regular FSA surveys of FBOs and consumers, we identified a need for more detailed evaluation metrics aligned with our theory of change.
We do not yet have budget confirmed for evaluative work, but will be bidding for 26/27 funding later this year. Subject to funding, we intend to:
- recommission both surveys in the summer of 2026 (post-guidance) to explore any changes in the baseline metrics and additionally measure awareness of the guidance. See Annex B for details of the survey methodology and sample. Post guidance surveys will have the same sampling quotas as baseline surveys.
- use pre-existing FSA surveys as interim measures. Appropriate survey questions will be added to our Small and Micro FBO tracking survey (in field November 25) and there are relevant existing FHS questions asked in wave 10 (pre guidance, winter 2024 fieldwork) and Wave 11 (post guidance, summer 2025) of Food and You 2.
- conduct qualitative research with FBOs ~18 months after publication of the guidance, to understand more about their experiences of following the guidance, challenges and best practices, and any unintended consequences.
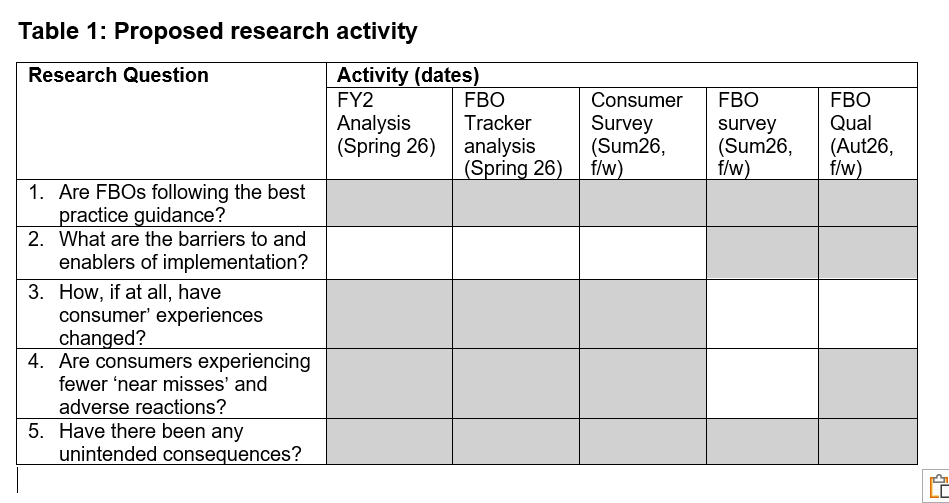
Table 1 shows how these activities map on to the 5 research questions.
Current evidence
This section outlines some key findings from the baseline surveys for each of the research questions (for consumers, baseline survey results are reported for adults with FHS only). It also draws on common themes in responses to the FSAs Consultation on Best Practice Guidance - Allergen Information for Non-Prepacked Foods[1], published in October 2024. A summary of responses is provided in the FSA response to this consultation.
RQ1: Are FBOs following the best practice guidance?
A key theme among FBOs who responded to the consultation and were supportive of the best practice guidance, was that they felt they were already doing what the guidance recommends. Our baseline surveys examined this claim in more detail, finding:
- 94% said their business currently provides written allergen information, either on its own or in conjunction with verbal allergen information. However, when asked to recall their most recent experience of buying non-prepacked food, 51% of adults with FHS said that the business provided written allergen information.
- 65% of FBOs surveyed said their business currently provides verbal allergen information to customers, either on its own or in conjunction with written information. Again, the number of adults with FHS who reported that allergen information was provided verbally the last time they bought non-prepacked food was much lower (38%). This suggests a potential barrier around initiating allergen conversations as consumers may not ask for it unprompted.
In follow up research, we are interested in exploring this gap between what allergen information FBOs say they provide versus what consumers get. 22% of adults with FHS said they couldn’t see allergen information and didn’t ask for it, which suggests a barrier around asking for and accessing written information.
- Businesses were asked how often they ask their customers if they have any allergies when customers are ordering food. Around half (52%) said they ask every time or most of the time. In line with this, when asked to recall the most recent time they bought non-prepacked food. the same proportion of adults with FHS (52%) said they were asked if they have a food allergy or intolerance before they ordered.
- When asked how staff and managers are provided with information and training on food allergens, only 1% of businesses said that they do not provide training. The most common types of training provided were:
- formal training for existing staff (46%)
- formal training for new staff (42%)
- online training (40%)
- updates given verbally to staff (38%)
- the Food Standards Agency allergen e-learning package (36%)
- FBOs were asked how they confirm allergen information when food is served, if a customer has made their allergy requirement known. 96% provide some kind of confirmation, including:
- 64% that confirm the allergen information verbally.
- 53% that include a label, flag or sticker with the food.
- Of those adults with FHS who made the food business aware of allergen requirements, 84% recalled getting confirmation that their allergen requirements when their food was served the last time they bought non-prepacked food:
- 38% asked their server to confirm this verbally.
- 34% said their server confirmed this verbally without being asked.
- 21% saw a label, flag, or sticker on their food.
- 7% said this was communicated some other way.
- When asked about providing written allergen information for takeaway orders:
- 30% of businesses said they provide a sticker or label on the food.
- 18% provide allergen information on their website.
- 15% provide it on a menu placed within the takeaway bag.
- 11% provide it via a QR code on the packaging.
- Over half (54%) of adults with FHS who ordered via distance sellers recalled being asked if they had a food allergy or intolerance before they ordered.
- Of those who made the food business aware of their food hypersensitivity, 88% of adults with FHS who ordered via distance sellers recalled getting confirmation that their allergen requirements had been met when their food was served. However, for the majority this confirmation was verbal rather than written:
- 45% asked their server to confirm this verbally.
- 33% said their server confirmed this verbally without being asked.
- 18% saw a label, flag, or sticker on their food.
- 17% said this was communicated some other way.
RQ2: What are the barriers to and enablers of implementation? How, if at all, have FBOs adapted their practices to follow the guidance, and what impact has this had on businesses?
We will add questions the FBO follow up survey to explore barriers to, and enablers of, implementing guidance. We will build on this with qualitative work with FBOs, following analysis of the survey results.
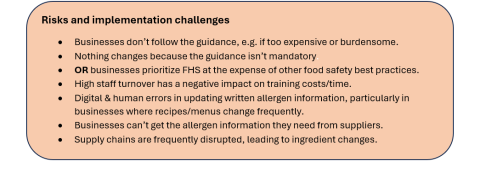
Potential barriers to implementation suggested in responses to the consultation on the draft best practice guidance included:
- The difficulty that some FBOs, particularly SMEs, could face in keeping written allergen information up to date, e.g. on printed menus.
- Relatedly, some FBOs, Local Authorities and trade associations highlighted supply chain challenges such as substitutions and product changes, and varying provision of ingredient information from suppliers. Again, this was highlighted as a particular difficulty for SMEs, who are more likely to have unstable supply chains and shop around on cost.
- Some FBOs and many Local Authorities opposed the emphasis on written allergen information, including enforcement officials who said this contradicts the best practice advice they give to SMEs and takeaway businesses.
- Conversely, some FBOs opposed the inclusion of allergen conversations in the guidance, in particular the recommendation that FBOs proactively ask their customers about allergens. They said this could lead to servers providing incorrect advice, and that they could not accommodate requirements beyond allergen-free menu items as listed.
- Consumers described instances of feeling too awkward or embarrassed to ask for allergen information, and some FBOs explained the difficulty of providing consumers with the information they need to make informed choices if they don’t make the business aware of their food hypersensitivity.
RQ3: How, if at all, have FHS consumers’ experiences of buying non-prepacked food changed since the introduction of the guidance?
Responding to the consultation, some consumers suggested that the provision of allergen information is already improving, but many also described challenges getting the information they need, including:
- Feeling awkward or embarrassed having to ask for allergen information.
- Being made to feel like a burden, or refused service, after disclosing FHS.
- Poor understanding of their allergen requirements from serving staff.
- Having to wait for a separate menu or allergen matrix.
They anticipated that if implemented, the best practice recommendations would give them more confidence eating out and the ability to make informed choices.
Whilst it may not be possible to attribute causality, it’s important that the evaluation explores access, confidence and trust as key intended outcomes of the guidance. The baseline consumer survey included metrics for each of these outcomes, which we will also include in the post-guidance survey. Relevant findings from the baseline survey include:
Access:
- Only 10% of adults with FHS said they are always able to get the information they need to help them identify ingredients that they avoid when buying non-prepacked food. 56% said they are able to get this information very often or nearly always, 29% said they are able to get this information less often, and 5% said they are never or hardly ever able to get this information.
- When asked about their general experience while eating out and getting takeaway in the last 6 months:
- 15% of adults with FHS said they have been refused service.
- 13% of adults with FHS said they have been asked to sign a disclaimer.
Confidence
- Adults with FHS had varying levels of confidence in their ability to avoid ingredients that they react to depending on how food is ordered, being most confident in eating a meal with table service (83%) and least confident in ordering takeaway over the phone (59%).
Trust
- Similarly, adults with FHS had varying levels of trust in different sources of allergen information, being most trustful of menus that list all ingredients for each dish (80%) and least trustful of digital menus on third party delivery websites/apps like Deliveroo or JustEat (58%).
RQ4: Are FHS consumers experiencing fewer ‘near misses’ and adverse reactions from non-prepacked food?
Whilst it may not be possible to attribute causality, it’s important that the evaluation explores this key intended impact of the guidance. The baseline consumer survey included metrics around near misses and adverse reactions, which we will also include in the post-guidance survey.
- When asked about their general experience while eating out and getting takeaway in the last 6 months:
- 42% of adults with FHS had at least one adverse reaction, where they became unwell after being served an ingredient that they react to.
- 34% of adults with FHS had at least one near miss, where they were served food containing an ingredient that they react to.
- When asked about their most recent reaction or near miss, 87% of adults with FHS said they had taken action to avoid this. Of this group, 60% had notified the business of their allergen requirements.
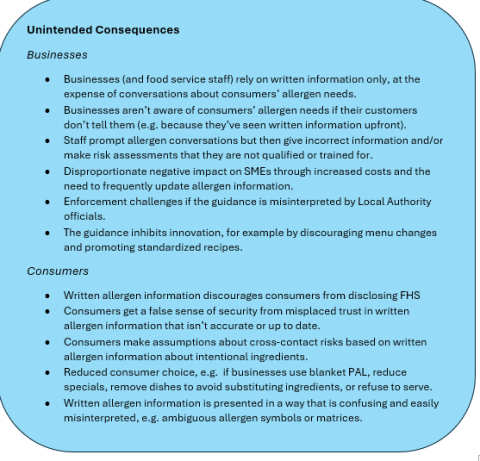
RQ5: Have there been any unintended consequences (positive or negative) for FBOs or consumers following the introduction of the guidance?
Consultation respondents were specifically asked a question about any unintended consequences that they thought might result from the best practice guidance.
- Negative unintended consequences that were common themes in their feedback included: the risk of consumers getting out of date or inaccurate allergen information; written allergen information discouraging conversations about allergen requirements, particularly if provided upfront; giving consumers a false sense of security; more precautionary allergen labelling as a blanket approach; reduced consumer choice; and additional costs for FBOs.
- Positive consequences that they mentioned included: improved accessibility and choice for consumers, more custom for FBOs, and the potential for written allergen information to improve FBO staff awareness.
We will add questions post-guidance to the FBO follow up survey to explore whether FBOs have experienced any of the unintended consequences identified in our theory of change. We also propose to build on this with qualitative work with FBOs.
The baseline consumer survey included metrics that we would hope to see improve following publication of the guidance. We are also monitoring these metrics in case there is a decrease (in which case, we would explore through qualitative work whether this indicates an unintended consequence of the guidance). These include:
- Consumers asking staff for allergen information
- Consumers disclosing their food hypersensitivity
- Consumers having a choice of venues and dishes when eating out
- FBOs asking consumers whether they have any allergies or intolerances
Additionally, the consumer survey is also monitoring the extent to which consumers come across precautionary allergen labelling when buying non-prepacked food.
[1] The consultation received 194 responses via an online form, and a further 19 by email correspondence, from consumers (n=70), FBOs (n=53), Local Authorities (n=39) and other stakeholders such as allergy charities, trade associations, and trading standards.
Qualitative and quantitative analysis of consultation responses was undertaken by FSA social scientists and economists. The FSA will publish its response to the consultation findings on the same date as the best practice guidance (5th March). This paper includes some headline feedback from the consultation as well as findings from the baseline surveys.
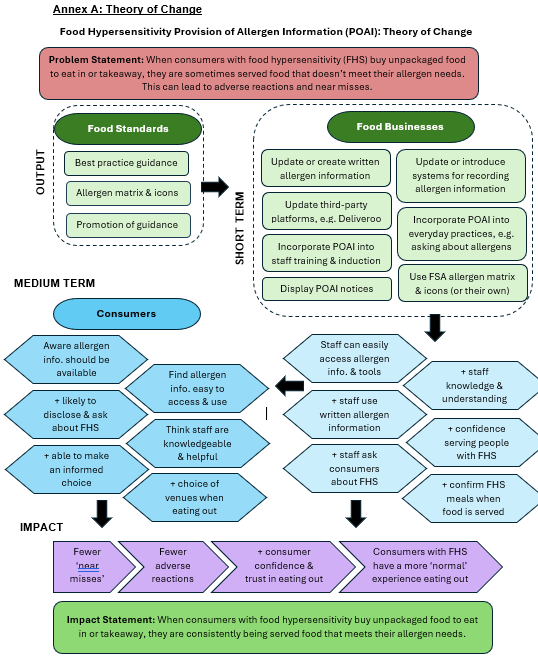
Annex A - Theory of change
Our theory of change model (Annex A) proposes that subject to FBOs implementing the key recommendations, there is the potential to influence all 3 of the key themes in the FSA Food Hypersensitivity Strategy: safety, trust and choice. Better communication of allergen information should enable consumers to make more informed choices, and subsequently lead to fewer near misses and adverse reactions, and increased consumer trust and confidence when eating out.
The theory of change proposes that for the best practice guidance to achieve this impact, we would expect to see:
- Short-term outcomes related to the key recommendations, such as FBOs creating or updating written allergen information, processes, and staff training.
- Medium-term outcomes such as improved FBO staff knowledge and routinisation of practices such as asking customers about allergens, providing written allergen information, and confirming allergen requirements when food is served. These medium-term outcomes would also be reflected in the consumer experience through improved access to allergen information and satisfaction with the information provided.
The theory of change also outlines underlying assumptions, risks, and potential unintended consequences of the best practice guidance. The guidance is based on previous FSA research on what works in the provision of allergen information, and it was written with the intention of mitigating the identified risks and unintended consequences. However, it is important that we monitor this as we evaluate the impact of the guidance and increase our understanding of the impacts.
19th March 2025 ACSS Plenary Meeting – Evaluating Allergen Information for Non-Prepacked Foods: Best Practice Guidance
Annex B: Baseline surveys
This Annex provides further information on the methodology and sample for the two baseline surveys of FBOs and food hypersensitive consumers. In each case, the surveys targeted respondents in England, Wales and Northern Ireland.
FBO survey methodology and sample
Opinium were commissioned to do an online survey of 520 Food Business Operators (FBOs). Fieldwork took place from 17th Jan – 7th Feb 2025. This was a brief survey that took approximately 5 minutes. Soft quotas we in place for business type, type of ownership (i.e. Independently owned, part of a chain), business size, and country.
Consumer survey methodology and sample
Ipsos-Mori were commissioned to do a survey of adults with a food hypersensitivity (n=780) and parents of children with a food hypersensitivity (n=184) to one or more of the 14 regulated allergens, about their experiences of buying non-prepacked food. Fieldwork took place from 13th December 2024 to 5th February 2025.
We intended to recruit participants from the Food & You 2 recontact sample, with an Access Panel boost for young adults aged 16-24. However, the recontact sample response rate was lower than anticipated (n=116). This meant in practice, Ipsos boosted via the Access Panel for all ages to recruit most respondents this way. Most respondents completed the survey online, but some of the Food & You 2 recontact sample were contacted by post. The survey took approximately 20 minutes to complete, and a small financial incentive was provided.
The final sample of adults with food hypersensitivity was weighted to the Food & You 2 profile of adults with a food hypersensitivity to one or more of the 14 regulated allergens, for key demographics (age, gender, country, ethnicity) plus severity of reaction. The sample of parents of children with a food hypersensitivity was not weighted because we do not collect this information directly in Food & You 2, and we could not identify another nationally representative dataset for this population. This difference in methodology between the two samples (representative and non-representative) means that results for adults with FHS and parents will be reported separately, and we cannot make direct comparisons between the two groups.
Analysis of this data is ongoing, so interim results in this paper are provided for the adults with FHS weighted population only. A full report, which we anticipate we will publish in spring/summer 2025, will include findings for both samples and analysis of key variables such as age, severity of reaction, and in-person vs. distance selling.